Multiple Sclerosis (MS)
Table of Contents

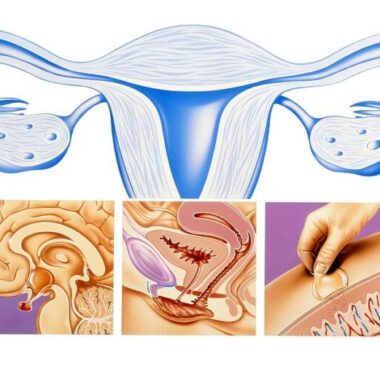
Multiple sclerosis (MS) is a chronic, complex, and often disabling disease of the central nervous system (CNS) with a variable clinical course. There are two basic forms of MS – relapsing/remitting and progressive. There is significant overlap between these two forms. Patients with MS have inflammation, demyelination, scarring of brain tissue, nerve cell degeneration, and dysfunction resulting from dysfunction of the immune system. Inflammation causing demyelination predominates in the relapsing remitting phase of the disease and is seen as recurrent episodes of worsening and improvement (exacerbation and remission). Neurodegeneratiion, leading to extensive brain nerve cell (neuronal) damage, occurs at the same time as the inflammatory process in progressive stages of the disease.
MS affects more than 2.1 million people worldwide and over 400,000 individuals in the United States, with about 200 new patients diagnosed every week. Although it can affect individuals at any age, MS is usually diagnosed between the ages of 20-40 years and is approximately 3 times more common in women than in men. As a leading cause of disability in young adults, MS substantially affects an individual’s quality of life and can cause a major financial and functional burden on the patient, family, and health care system.
SIGNS AND SYMPTOMS OF MULTIPLE SCLEROSIS
The main symptoms of MS can vary by patient and may change or fluctuate over time. For many years MS has been considered a white matter disease (i.e., involving sensory and motor findings). Magnetic resonance imaging (MRI) has allowed us to see that MS lesions occur in grey matter too (i.e., involves cognitive behavior), leading to a wider range of complex neurologic symptoms.
Some of the more common symptoms may include varying degrees of vision problems, fatigue, paresthesia, bladder/bowel/sexual dysfunction, gait problems, spasticity, dizziness/ vertigo, pain, depression, and cognitive dysfunction. Less common symptoms may include headache, hearing loss, seizures, tremors, incoordination, and speech and swallowing difficulties. These symptoms may lead to additional secondary complications, e.g., urinary tract infections, loss of muscle tone, decreased bone density, shallow breathing, pressure sores, and tertiary, e.g., social, vocational, and psychological complications, which create their own challenges to effectively treat and manage.
Because MS is diagnosed at a relatively young age (20 to 40 years), and continues to evolve over time, it causes a greater economic burden than many other chronic diseases over the lifespan of the individual and has a huge impact on health, quality of life, productivity, and employment over many years.
TRADITIONAL THERAPIES
No one knows what causes MS. It is influenced by multiple interacting genetic, environmental, nutritional, hormonal, and viral factors. It is also correlated with geophysical parameters, such as sunshine exposure and variations in the Earth’s magnetic field, both of which are a function of location and seasonal influences.
Treatment of MS has advanced significantly over the past several decades. Historically, MS treatment was mostly supportive in decreasing the severity of exacerbations (MS attacks), relying on short-courses of powerful steroids. In the 1990s disease-modifying therapies (DMTs) began to be used for long-term treatment, to proactively manage and retard disease progression. While DMTs have benefits in reducing the occurrence of relapses and future disability, they can have important side effects. Despite their popularity and heavy reliance with doctors, they do not work equally well in everybody, reducing relapse rates only by only about 30%.
There is no consensus as to which DMT should be used for what type of MS patient. There are no studies that have evaluated which therapies are most appropriate for a particular MS patient group. The benefits of typical DMTs happen over long periods of time, typically beyond 4 years. This is another reason why new options for shorter term therapies are necessary for the comprehensive and total management of MS.
Generally, treatment with traditional therapy is considered relatively safe. The most frequently adverse effects include: injection-site reactions, flu-like symptoms, fatigue, muscle pains, elevation of liver enzymes, blood abnormalities, fat atrophy, infections, post-infusion reactions, and progressive multifocal encephalopathy (PML)- an often fatal demyelinating disease of the central nervous system. PML has been confirmed among 104,300 patients treated with natalizumab, 62 being fatal. Mitoxantrone may cause therapy-related acute leukemia and cardiotoxicity.
Fingolimod can lead to cardiac abnormalities such as slow heart rate and heart block, hypertension, liver and respiratory changes, infections, and macular edema. Teriflunomide and leflunomide may cause diarrhea, elevated liver enzymes, nausea, flu-like symptoms, and thinning or loss of hair, embryo-lethal effects in some animals. BG-12 has been associated with flushing (30%-40%) and gastrointestinal symptoms (e.g., diarrhea, nausea/vomiting, abdominal pain; about 20%). Alemtuzumab may cause hyperthyroidism and auto-immune thrombocytopenic purpura (ITP), and increased risk for super-infections and cancers.
So, given all these limitations of current approaches to managing MS, this is yet another reason that new approaches are needed.
MAGNETIC FIELD THERAPY AND MULTIPLE SCLEROSIS (MS)
In the search for other therapies to help manage MS, I have become aware of the potential for pulsed electromagnetic fields (PEMFs) to impact neurological tissue at a fundamental level. While there is little evidence at this time to suggest that PEMFs may actually be able to reduce plaque size, there is some suggestion that there is a possibility that PEMFs may be able to reduce recurrences and perhaps delay progression of MS as well.
Research suggests that PEMFs – although not a cure – can alleviate many of the major symptoms of MS, including spasticity, fatigue, cognitive function, mood changes and other impaired physiologic functions. This is because PEMFs act at such basic cellular and physiologic levels. They improve the function of all cells of the body, even those impaired by any specific disease process, such as MS. As such, PEMFs can substantially enhance the quality of life of individuals with MS without the side effects associated with pharmaceutical approaches.
Because every molecule, cell, organ in our body emits and is sensitive to electromagnetic fields, our biochemistry is influenced by our electromagnetic nature. As such, efforts to develop new therapies based solely on dysfunctional biochemistry without considering this nature ultimately will be limited. It is like replacing worn auto tires without aligning the wheels that caused the tires to get worn in the first place, i.e., you need to tackle both problems, so they don’t recur.
Although there is no tissue in which our electromagnetic nature is more evident than MS-attacked nervous tissue, most therapeutic efforts have emphasized the disease’s overt physical symptoms associated with demyelination. They also minimized, until recently, the role of its less understood, underlying electromagnetic dynamics.
Electromagnetic fields influence many biochemical and physiological processes. Although the specific mechanisms by which such fields alleviate MS symptoms remain undefined, many possibilities exist. For example, through influencing the flow of charged ions through membrane-transversing, protein channels, electromagnetic fields may enhance signal conduction in dysfunctional neurons. In another example, magnetic fields alter our neuro- and immunochemistry, both of which are affected by MS.
Electromagnetic fields influence the levels of various MS-altered hormones. Dr. R. Sandyk (Touro College, NY) has intriguingly suggested that a key player in the disease’s etiology is the brain’s all-important, magnetically and light-sensitive pineal gland, which secretes hormones (e.g., melatonin) that affect the entire body (J. Alternative & Complementary Medicine, 1997; 3(3): pp 267-290).
The epidemiology, pathogenesis, clinical manifestations, and disease course of MS can all be correlated with the pineal gland. For example, most individuals with MS have calcified (i.e., dysfunctional) pineal glands. If MS demyelination is a secondary consequence of pineal dysfunction, Sandyk believes research efforts should focus on therapeutic interventions, such as magnetic therapy, that enhance pineal functioning. [Interestingly, quadriplegics, but not paraplegics, also have dysfunctional pineal glands (Zeitzer JM et al. J. Clinical Endocrinology & Metabolism, 2000; 85(6): pp 2189 –2196)]
Magnetic field therapeutic interventions reviewed below use PEMFs in which an electromagnet is turned on and off at a defined frequency. For example, a field that is pulsed 25 times per second has a frequency of 25 cycles/second or Hertz.
Field strength is defined by gauss. For reference, the Earth’s magnetic field is about 0.5 gauss, a refrigerator magnet is about 10 gauss, and some medical applications, such as MRIs, can exceed 10,000 gauss. However, because size counts, the Earth’s low intensity, large size, field profoundly influences life, including MS expression. The following studies use weak electromagnetic fields, which scientists believe can initiate physiological responses that much stronger fields often cannot. These researchers have postulated a “window effect,” in which these responses may only be initiated at a unique combination of frequency, intensity, and polarity relative to the Earth’s magnetic field.
But despite the theories, is there evidence that PEMFs affect brain function? Behavioral and neurophysiological changes have been reported after exposure to extremely low frequency magnetic fields (ELF-MF) both in animals and in humans. Even in the nonliving human neuronal cultures exposed to extremely low frequency PEMFs show an increase in excitatory neurotransmission. Excitatory neurotransmitters turn functions on, and inhibitory neurotransmitters reduce functions.
Using transcranial brain stimulation, Capone studied noninvasively the effect of PEMFs on several measures of cortical excitability in 22 healthy volunteers, and in 14 sham field exposure was used. After 45 min of PEMF exposure, intracortical facilitation function related to cortical glutamatergic activity was significantly enhanced by about 20%, while other parameters of cortical excitability remained unchanged. Sham field exposure produced no effects. This study shows some indication that PEMFs can produce functional changes in human brain.
There is growing evidence in the literature of the beneficial effects of magnetic fields on different MS symptoms. Guseo reported that the technique can alleviate symptoms such as fatigue, bladder control, and spasticity, as well as improve quality of life. Richards et al. performed a double-blind study to measure the clinical and subclinical effects of a magnetic device on disease activity in MS and showed that a magnetic field improved the performance scale (PS) combined rating for bladder control, cognitive function, fatigue level, mobility, spasticity, and vision. Nielsen et al. showed in 38 MS subjects that magnetic stimulation on spasticity could improve self-score of ease of daily activities and clinical spasticity.
Regarding fatigue, commonly seen in MS, Sandyk proposed that depletion of neurotransmitter stores in damaged neurons may contribute significantly to the development of fatigue and showed that a picotesla PEMF in a small group of MS subjects improved fatigue. These results suggestedthat replenishment of neurotransmitter stores in neurons damaged by demyelination in the brainstem by periodic applications of picotesla PEMFs may lead to more effective impulse conduction and thus to improvement in fatigue.
Another possibly related way pulsed PEMFs might remediate MS fatigue is through electrophysiological effects. Richards et al. found that in MS patients, during a language task and after visual stimulation, EMFs increased the amount of brain alpha activity. G. Another study showed significan positive t differences in theta and beta band amplitudes between subjects exposed to real and sham 3 Hz magnetic fields (Heusser).
VERY LOW INTENSITY PEMFS
Sandyk (1998) found that transcranial applications of pico Tesla AC PEMFs produced rapid and sustained improvement of symptoms in patients with chronic progressive or secondary progressive MS, and evidence of normalization of electrophysiologic evoked potential responses. He further discovered recurrent episodes of uncontrollable yawning and body stretching, identical to those observed upon awakening from physiological sleep. This behavioral response has been observed exclusively in young female patients who are still fully ambulatory with a relapsing remitting course of the disease.
This is a distinctly favorable therapeutic response to magnetic stimulation. This response is likely due to the production of adrenocorticotropic hormone (ACTH) stimulated by the PEMFs. There is support for this possibility in other research. Intracerebral administration of adrenocorticotropic hormone (ACTH) in experimental animals elicits yawning stretching behavior. A surge in plasma ACTH levels at night and just prior to awakening from sleep is also associated in humans with yawning and stretching behavior. In addition, ACTH is sometimes used to treat MS due to its immunomodulatory effects.
Sandyk (1997) describes the use of PEMFs in a woman with chronic progressive (CP) MS. A 40 year-old woman presented in December of 1992 with CP MS with symptoms of spastic paraplegia, loss of trunk control, marked weakness of the upper limbs with loss of fine and gross motor hand functions, severe fatigue, cognitive deficits, mental depression, and autonomic dysfunction with neurogenic bladder and bowel incontinence. Her symptoms began at the age of 18 with weakness of the right leg and fatigue with long distance walking and over the ensuing years she experienced steady deterioration of functions. In 1985 she became wheelchair dependent and it was anticipated that within 1-2 years she would become functionally quadriplegic. In December of 1992 she began experimental treatment with pico Tesla PEMFs.
While receiving regular weekly transcranial PEMF treatments over the next year, she experienced improvement in mental functions, return of strength in the upper extremities, and recovery of trunk control. During the second year she experienced the return of more hip functions and recovery of motor functions began in her legs. For the first time in years she could initiate flexion of her ankles and actively extend her knees voluntarily. Over the next year she started to show signs of redevelopment of gait. With enough function restored in her legs, she began learning to walk with a walker and was able to stand unassisted and maintain balance for a few minutes.
She also regained about 80% of the functions in her upper limbs and hands. Most remarkably, there was no further progression of the disease during the 4 year course of magnetic therapy. This patient’s clinical recovery cannot be explained on the basis of a spontaneous remission. He suggested that pulsed applications of PEMFs affect the neurobiological and immunological mechanisms underlying the pathogenesis of CP MS. but, these regenerative changes in the brain require a long course of treatment, possibly forever.
During his extensive experience in treating MS with PEMFs Sandyk also saw the resolution of sleep paralysis and diplopia, reversal of alexia, , improved bladder and the swallowing function, resolution of the Lhermitte’s sign, and reversal of abnormal evoked potentials, indicating improvement of electrophysiologic functions.
The best results appeared to occur in people who had the longest courses of care. There appeared to will be a lack of correlation between the extent of demyelinating plaques on MRI and the rate and extent of recovery in response to PEMFs. These results suggest that the dysfunction of brain cell connectivity due to neurotransmitter deficiencies contribute more significantly to the development of MS symptoms than the process of demyelination, which may clinically represent a side product of the disease.
MEDIUM INTENSITY PEMFS
Guseo has conducted a number of double blind controlled experiments using an 8 milliTesla PEMF device at 2 or 50 Hz for 20 minute treatments applied to either the head, trunk or thighs. All the treatment subjects experienced improvements in circulation. In a separate study, patients were given 15 daily treatments or sham-treatments in a reclining or sitting position by placing the coil on the upper and lower spine areas, then on the lower extremities. The applied magnetic waveform was a 300 Hz sine wave with repetition rates of 2-50 Hz. The peak applied magnetic field strength was 5-7 mT. In addition to the patients in the double-blind study, 104 patients were treated in an open series involving one or more groups of treatments, each grouping separated by 3 or more months, for up to 5 treatment series over a period of 18 months.
Patients in the placebo group of the double-blind study got an open series of treatments after 1 month and were termed a crossover treatment group. Double-blind results showed “well improved” or “improved” status for 7/10 PEMF-treated patients, and only 2/10 of the placebo group. In the open series, 83/104 were “well improved” or “improved”, as were 8/10 of the crossover group of former placebo patients. The improvement in most cases made everyday life easier: general weakness improved, walking longer distances or stepping on stairs became possible, and bladder incontinence improved in 26/50 patients with urinary incontinence. A notable effect of the PEMF was to reduce spasticity and pain.
Wieczorek, using the Guseo’s method, treated 126 MS patients, who mainly had spastic syndromes. 50-60% of the patients reported a favorable effect of the therapy with spasticity, vasomotor headache, and spinal pain.
Mix studied 10 patients with MS using a similar system. Treatments consisted of 20 daily exposures of low-frequency (10 Hz) PEMF for 15 min. Clinically, 30% of their MS patients had immediate subjective improvement.
Terlaki treated 97 patients with multiple sclerosis (MS) over a 3-yr period, 7 had MS with associated disorders. Most of the patients were treated while in the hospital. They received a total of 177 courses of PEMF therapy using the Gyuling-Bordacs (GB) magnetotherapy device. A typical course consisted of 10-25 treatments administered daily, 6 days/wk. Health status improved, worsened, or remained unchanged. 21% had no benefit . In 6% of the cases the condition deteriorated or treatment was interrupted for some reason. 73% showed some improvement. I 42 of 54 female MS patients (78%) and 25 of 43 male MS patients (58%) reported improvement after their treatment series.
Five MS patients with urinary incontinence reported improvement. In several patients, muscle spasticity decreased to such a degree that the dose of muscle relaxants could be reduced or even discontinued. Most of the other MS patients reported increases in muscle strength. No permanent adverse side effects of the treatments were seen. No precise data on how long the benefits from treatments lasted were available, but a few patients reported benefits lasting for 3-7 months. Full recovery was not seen with this short course of treatment in these more severe MS patients, as one might expect.
Another group (Brola) undertook a study using a low to medium intensity PEMF system. They included 76 patients with a long-term history of clinically confirmed MS, mean duration 8.5 years, and mean age of 37.8 years. The patients were divided into two groups: the study group and non-treated controls. Study group patients were exposed to sinusoidal PEMFs, 1-10 mT, 20-50 Hz. Standardized instruments of function were assessed on admission and after 21 days of stimulation.
No significant differences between the groups were found with motor impairment.Quality of life was found to be significantly better in the PEMF group than in the controls (p < 0.01). The most significant difference was seen in the mental state of the patients (alleviation of depression, elimination of anxiety, better emotional control), as well as decrease of muscle tone, altered sensations and pain. No side effects were seen . The authors concluded that PEMF therapy may supplement symptomatic treatment of patients with multiple sclerosis.
HIGH INTENSITY PEMFS
High intensity PEMFs, using rapid transcranial magnetic stimulation (rTMS), have been studied in MS. Using PEMF stimulation over the scalp, currents can be induced within the brain to excite the motor cortex, even to the extent that the brain would cause intended muscles to contract. Mills found that after a cortical stimulus spinal neurons controlling muscles are induced to fire by sending impulses over fast conducting spinal nerve fibers.
Nielsen used high intensity TMS on spasticity in 38 patients with multiple sclerosis in a double-blind placebo-controlled study. The maximum field intensity was 1.2 T, placed in the midline of the back of the chest with the bottom part of the coil placed over the 8th thoracic vertebra. One group was treated with intermittent repetitive magnetic stimulation (n = 21) for 25 minutes and the other group with sham stimulation (n = 17). Both groups were treated twice daily for 7 consecutive days. They evaluated changes in the patients’ self-score, clinical spasticity score, and in the stretch reflex threshold.
The clinical score improved by 18% [P= 0.003] after treatment and was unchanged in the sham group. The self-score of ease of daily day activities improved by 22% (P = 0.007) after treatment and by 29% (P = 0.004) after sham stimulation. The clinical spasticity score improved in treated patients and improved less or worsened with sham stimulation (P = 0.003). The stretch reflex threshold increased by 27% in treated patients and remained unchanged in the sham group. In the treatment group 50% of the patients improved their self score, 70% their clinical score and 50% their stretch reflex threshold. In the placebo group 59% improved their self score, 59% improved clinical scores and 29% improved the threshold of the ankle stretch reflex.
The effects lasted at the same level for 24 hours. 8 days after the end of treatment the stretch reflex remained improved by 27% in the treatment group as compared to baseline. After 16 days no statistically significant effect of treatment could be detected. The data presented in this study supports the idea that repetitive magnetic stimulation has an antispastic effect in multiple sclerosis. These results are comparable to the success rates of pharmacotherapy. Many MS patients who need to moderate spasticity cannot tolerate or refuse medication treatment because of side effects. TMS is well tolerated with no significant side effects. Transient dizziness was the primary side effect, thought to be due to blood pressure changes . The author recommended placement lower down on the spine than used in the study. TMS appears to be more tolerable than electrical stimulation since there is no induced pain or muscle contractions.
Spasticity in MS was also studied by a different group (Centonze). They used high-frequency (5 Hz) and low-frequency (1 Hz) rTMS protocols in 19 remitting patients with relapsing-remitting multiple sclerosis and lower limb spasticity. A single session of 1 Hz or 5 Hz rTMS over the leg primary motor cortex improved ankle stretch reflex. Single sessions did not induce any effect on spasticity. Improvements of lower limb spasticity were better when rTMS applications were repeated over a 2-week period. Clinical improvement was long-lasting (at least 7 days after the end of treatment) when the patients underwent 5 Hz rTMS treatment during a 2-week protocol. No effect was obtained after a 2-week sham stimulation.
With regard to safety of high intensity PEMFs, one study was done to evaluate the effects of rTMS on the permeability of the blood-brain barrier (BBB). In contrast to magnetic resonance imaging (MRI) in which the subject is exposed to static magnetic fields superimposed with small PEMFs , rTMS uses a large number of powerful, short duration pulses. MRI has been reported to increase the permeability of the BBB in rats. The rTMS treated rats received 50 stimulations a day for one week and compared to unexposed controls. Each stimulation session lasted 10 minutes, peak intensity of 1.9 T. BBB permeability was assessed in mid-frontal, mid-parietal and mid-occipital cortices, the cerebellum and the midbrain. The results revealed no significant differences in any of the five brain regions. The authors concluded that transcranial pulsed magnetic stimulation can be regarded as safe with regard to blood-brain barrier integrity.
Using rTMS 5-Hz over the motor cortex in people with multiple sclerosis (MS) with cerebellar symptoms appears to improve hand dexterity (n=8) but does not change dexterity in healthy subjects (n=7) (Koch).
Another group (Centonze ) tested the effects of 5-Hz rTMS over the motor cortex in individuals with MS complaining of lower urinary tract symptoms either in the filling or voiding phase. Motor cortex stimulation for five consecutive days over two weeks improved the voiding phase of the micturition cycle, suggesting that enhancing spinal excitability might be useful to improve bladder contraction and/or urethral sphincter relaxation in MS patients with bladder dysfunction.
While there is plenty of evidence to suggest that PEMFs may be very helpful in MS for a wide range of symptoms and functional limitations, there is at least one study demonstrating a lack of benefit for fatigue in MS. 50 MS subjects with primary fatigue were evaluated in a randomized double-blind cross-over trial (de Carvalho), recruited at a rehabilitation center, in Italy. Patients were randomized into two groups: magnetic field group and sham therapy group and evaluated with a fatigue impact scale, fatigue severity scale, VAS and 10 m walking test.
Each group received both sham therapy and magnetic field therapy for 24 min per session, three times per week, for 8 weeks with a wash-out period of 5 months. Patients had a statistically significant improvement in physical scores (p < 0.05). Using this particular PEMF system, the researchers found no significant benefits for fatigue, despite improvement in physical function. Lack of obvious benefits of PEMFs for fatigue in MS can be related to the particular PEMF system or the research design that incorporated this particular PEMF system. Often studies are not carried out long enough with devices that do not have a sufficient magnetic field intensity to produce results within the parameters of the study.
SUMMARY
MS is a complex disorder for which there is no cure. Existing medical therapies delay the progression and severity of the condition. They do virtually nothing for the existing symptoms and damage caused to the nervous system. Because MS can be such a disabling condition, and because medical therapies are so focused on delaying progression, people suffering with symptoms from their condition have few helpful alternatives to their current state. As I have indicated many times before, PEMFs are not a panacea. People with various medical conditions require a teamwork approach to resolve their health issues.
Although the reviewed PEMF studies in MS demonstrate positive outcomes overall, they have somewhat varied outcomes individually, which could be due to the specific device, the study design, sample size (e.g., more subjects may statistically demonstrate subtler effects), treatment duration, type of MS, medication history, etc. Therefore, selecting an appropriate PEMF system will require some degree of expertise, preferably with the assistance of a medical professional very familiar with PEMF therapies.
The good thing about the above review, is that there is evidence to indicate that PEMFs of various intensities and designs may all facilitate various aspects of dysfunction and disability associated with MS. Low intensity PEMFs would generally be expected to produce their results over a longer period of time. High intensity PEMFs, with multiple courses of multiple treatments, can produce enduring results for variable periods of time beyond therapy, up to several weeks or months after treatment.
Because MS is a chronic, long-term, lifelong, progressive condition, it is normally recommended that individuals own a whole body home care therapeutic PEMF system of sufficient intensity, which can be used daily to regularly stimulate underlying neurological and physiologic functions in the whole body, all of which may be compromised by the MS process. It’s probably also advisable to periodically have access to a professional high intensity therapeutic system, if locally available.
It’s also likely that no one system is going to do everything that may be needed to help to control the spectrum of MS dysfunctions. For this reason, good nutrition, exercise, healthy lifestyle, supplements, herbs, acupuncture, chiropractic, guided imagery, mind-body approaches and other body therapies can still be very helpful , all used together.
Using PEMFs does not mean that DMT’s shouldn’t be tried. It is very probable that the combination will actually be much more effective, as is seen in the management of many health conditions. In addition, other immune therapies, such as low dose naltrexone (LDN) or even the cannabis-based therapies with high concentrations of cannabidiol [CBD], as they become available in various states in the United States, would also be complementary to the use of PEMFs, enhancing the effects of both.
Cumulatively, the studies reviewed here present support that electromagnetic PEMF therapy has considerable potential for expanding the healing spectrum of people with MS.