Management of Neurological Disorders
Table of Contents

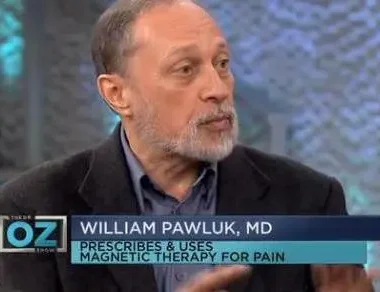
This October, Dr. Pawluk appears on the cover of Townsend Letter. Townsend Letter, the Examiner of Alternative Medicine, publishes a print magazine about alternative medicine. It is written by researchers, health practitioners and patients. In the October issue of this magazine, he shares extensive research and references on PEMF (Pulsed Electromagnetic Field) Devices in the Care and Management of Neurological Disorders.
PEMF (pulsed electromagnetic field) devices chiefly reflect an emerging approach to cost-effective therapy for difficult-to-manage neurological and pain disorders. The primary focus of this review is the use of devices of low electromagnetic intensity and frequency, designed for self-care by consumers, with assessment, guidance, and follow-up by their clinicians.
Indications. PEMF for neurological disorders has been shown to support progress in neuro-chemical conditions that include addiction, ADHD, anxiety, autism spectrum disorders, depression, PTSD, and sleep issues. Research also indicates benefit for neuro-pathologies such as concussion, memory loss, mild cognitive impairment (MCI), mild traumatic brain injury (TBI), multiple sclerosis, Parkinson’s disease, stroke, and tremor. (A variation of PEMF, high-powered rTMS (repetitive transcranial magnetic stimulation) devices used in hospitals are FDA-approved to treat conditions ranging from bone healing to resistant major depressive disorders (MDD).
Mechanisms of action. As a magnetic field passes through the body, that field can stimulate a range of potential processes and activities, depending on the frequency and power:
- Reducing inflammation and edema (Jerabek & Pawluk, 1996)
- Increasing ATP production (Ascherl, Blumel, Lechner, et al., 1985; Blank & Soo, 1992; Chen, Cui, Yue, et al, 2009)
- Rebalancing circadian rhythm (Manzella, Bracci, Ciarapica, et al., 2015)
- Improving circulation and blood supply (Bartko, Turcáni, Danisová, et al., 1988)
- Increased oxygen to the body’s tissues (Warnke, 1992; Grant, Cadossi, & Steinberg, 1994)
- Healthy levels of growth factors and nitric oxide (Goodwin, 2003)
- Increasing cell metabolism (Jerabek et al, 1996)
- Production of endogenous antioxidants (Singh, Khanduja, & Mittal, 1998)
- Enhanced detoxification (Singh & Khanduja, 1998)
- Wound healing and tissue regeneration (Blackman, 1988; Blank & Soo, 1992)
- Stimulating and rebalancing the immune system (McEver & Zhu, 2010)
- Improved nerve conductivity and regeneration (Polk, 1992)
- Promotion of growth gene factors (Goodwin, 2003; Lagrove, Bersani, Billaudel, et al., 2003)
- Support of neural stem cell production (Li, Zhao, Xing, et al., 2002; Goodwin, 2003)
- Reduced pain (Nelson & Esty, 2009, 2015)
- Autophagy (Marchesi, Osera, Fassina, et al., 2014)
- Enhanced neurotransmitter levels (Zecca, Margonato, & Esposti, 1989)
- Effect on monoamine function (Sieron, Labus, & Nowak, 2004)
- Reduced reaction time (Blackman, 1988)
- Charge displacement from neuronal membranes of cortical neurons (Persinger & Saroka, 2013)
OVERVIEW ON DEVICES
Pulsed electromagnetic devices encompass a broad range of appliances with corresponding capabilities.
High-intensity, high-frequency devices utilized in health systems. In terms of high-end devices, a robust literature is available, documenting approximately 2,400 clinical trials using rTMS to date. rTMS devices operate at an intensity of 8,000 gauss. By way of context, an MRI machine produces a high-intensity magnetic field ranging from 20,000 to 60,000 gauss (2 to 6 Tesla) depending on the machine and application. rTMS devices have been approved since 2008 and are reimbursable for the treatment of medication-resistant depression.
These units cost approximately $50,000, so they are typically found in hospital medical centers and large mental health group practice. rTMS enhances neuroplasticity, entrains and resets brain cell oscillators between the thalamus and the cortex, normalizes regulation, facilitates reemergence of natural cerebral rhythms, and through these mechanisms restores normal brain function. TMS can be administered broadly at a lower magnetic field strength to treat multiple brain areas simultaneously.
Low-intensity, low-frequency devices for self care. Additionally, At the other end of the spectrum are devices designed for home use and self-care, currently in the range of $500 to $13,500. The frequency of these devices is typically 1 to 100 Hz, (454) with intensity ranging from 70-7,000 gauss, and typically used to support sleep, pain management, or numerous other aspects of healing. Electronic appliances for consumer use are typically in the range of extremely low frequency (ELF) at or below 1,000 Hz.
Consequentially, the therapeutic process focuses on given brain wave states (gamma, beta, alpha, theta, and delta). These are scientifically well known and frequency-specific. Ninety years of brain imaging have made it clear that the brain is an organ which responds to frequency. Alpha and beta brainwaves are produced by the brain itself. They were first reported in the medical literature in 1929 by the German neurologist, Hans Berger, the inventor of the EEG. Since that time, frequency states of the brain have been measured and associated with a range of mental states and activities–alpha through gamma.
In meditation, a great deal of research exists for use of magnetic field frequencies. This is used to achieve the same brainwave entrainment using the theta frequency (4 to 7.5 Hz), or the more recently discovered 40 Hz gamma. In contrast, a PEMF signal within the beta range (from 13 to 25 Hz) provides an overall effect of increased alertness by typically causing a greater portion of the brain to synchronize with that frequency.
Basically, brainwave entrainment is the practice of causing brain waves to fall into step with an external stimulus. Neurofeedback, for example, seeks to entrain the brain by promoting these frequencies. However, as a clinician, I personally stopped providing neurofeedback. Consequentially, because I found that magnetic field therapy could do the job faster than neurofeedback, which tends to be slow and costly to patients.
More powerful PEMF systems are designed for use in the clinical environment by providers for therapeutic interventions. These include pain management and rely primarily on higher density pulses rather than frequency. A PEMF will pass completely through the body whether it is of high or low intensity. The difference is the amount of charge the field will stimulate in the tissues as it moves through the body. This is based on Faraday’s law. The magnetic fields produced by the body itself are well under 1 thousandth of a gauss (nano- or pico-Tesla), or less than one tenth of a microTesla. Human biology is affected by and responds to a vast range of magnetic field intensities.
Differentiating PEMF from EMFs. There are EMFs produced by cell phones, microwave appliances, cell towers, and Wi-Fi. They all involve extremely high frequencies, with very short wavelengths. They are are absorbed by the body, with the potential for damage. In contrast, ELF (extremely low frequency) PEMF devices are extremely low frequency with extremely long wavelengths; therefore, they penetrate through the body completely and do not stop in the body. The body is transparent to extremely low-frequency magnetic fields.
| Electromagnetic Frequencies | |
| Static electric or magnetic fields | 0 Hz |
| Extremely low frequency (ELF) electric or magnetic fields | 1 – <300 Hz |
| Delta, theta, alpha, beta, gamma frequencies | 0.1–100 Hz (200 gauss or greater) |
| rTMS treatment | 1-20 Hz (8,000 gauss) |
| Intermediate frequency electromagnetic fields | 300 Hz – 100 kHz |
| High Frequencies | 100 kHz – 10/30 THz |
|
Radiofrequency electromagnetic fields (radiowaves), Microwave ovens – 100 MHz |
100 kHz – <300 MHz |
| Microwave radiation | 300 MHz –<30 GHz |
| Wi-fi communications— | 900 MHz – 60 GHz |
| 5G Millimeter waves (MMW) | 30 GHz – <300 GHz |
| Terahertz waves | 300 GHz – 10/30 THz |
Table 1. The range of electromagnetic frequencies in medicine, manufacturing, and communications.
CONTRAINDICATIONS AND SAFETY
Patients with a pacemaker or other type of implanted electrical device. The only absolute contraindication for use of a PEMF device is the caution not to place an active applicator over an implanted electrical device such as a pacemaker, cochlear implant, intrathecal pump, etc., because the magnetic field can shut off the device or otherwise interfere with its function. There are increasingly available MR-conditional implanted electronic devices that are safe with PEMFs.
Organ transplant patients. PEMF therapy is also contraindicated for these patients, since they take immune suppression medications to prevent organ rejection. There is a chance that PEMFs may actually stimulate or activate a more aggressive rejection process by stimulating the immune system. PEMF interactions with immunosuppressive medications can be unpredictable.
Implanted metals. Extremely high intensity PEMFs should be used with caution or with professional guidance for people with implanted metals, such as joint replacements, dental implants, mechanical heart valves, metal stents, or metal staples, because extremely high intensity PEMFs may stimulate the nerves in the area of the metal, causing sharp pain.
Pregnancy. Although there is no evidence of harm, the safety of PEMFs has not been proven in pregnancy.
Bleeding or Grave’s disease. PEMFs should be used with caution in Grave’s disease or in the case of active bleeding.
Seizures. There is now a fairly large body of research regarding the use of PEMFs of different intensities and the potential association with seizures. Evidence indicates that PEMFs are very unlikely to cause seizures, based on research studies using high-intensity PEMF systems, which have the highest concern for generating seizure activity. In fact, studies have suggested that PEMFs are capable of providing benefit to epileptic patients (Menkes, 2000). In a study of 58 patients with partial or generalized epilepsy, TMS did not provoke seizures or EEG changes in any patient. Long-term follow-up found that their epileptic conditions were not made worse by TMS. Subsequently, a review of 20 studies involving 859 subjects found that 45% of patients responded favorably to treatment and 28% experienced seizure cessation.
Adverse effects. Most adverse reactions are mild and temporary and can be managed by simply continuing the therapy. Sudden increases in circulation, especially in ischemic tissues (areas with restricted or reduced blood flow) may lead to uncomfortable increases in circulation for a short time after the magnetic field has been applied. The increase in circulation, while usually a desirable effect, can lead to a surge of oxidative stress. It is desirable to have adequate antioxidant support in the body before beginning treatment. Sudden improvements in circulation may also lead to aggravations of existing extensive or severe inflammatory processes, typically in the skin or soft tissues.
Aggravation of hives is likewise possible and should be considered before starting treatment. In individuals with electrical hypersensitivity and electromagnetic hypersensitivity, these reactions are more common and more uncomfortable. However, rarely does magnetic therapy have to be discontinued as a result. The recommendation is to use lower intensities and shorter treatment times.
If the adverse reactions are intolerable, they can be lessened by making small changes to the protocol. These changes include lowering intensity, and decreasing treatment times. These changes should only be necessary on a short-term basis since reactions tend to diminish relatively quickly with continued treatment and as healing progresses.
PEMF IN CLINICAL PRACTICE
The problem with being prescriptive or instructive on the use of a PEMF device is that it depends on the specific PEMF system. PEMF in clinical practice means first, understanding the instrument you are utilizing, and how PEMFs work. You must also understand the pathophysiology that you’re dealing with, and the therapeutic potential of the device for that disorder. Essentially this is a process of putting two and two together. There are many PEMF systems and every system is going to have a particular aspect of how you would use it.
Begin with low intensity and brief treatment times. Observe the patient’s response. If they are progressing in the desired direction, increase the time and intensity in increments. Once the patient is stable in their response, it becomes a matter of healing the brain, to the extent that it can be healed, and then moving into maintenance mode to maintain the benefit.
Frequency. Frequency is literally a measure of the frequency of the pulsing of a particular magnetic field. Typically, a single frequency is selected and with the continued stimulation, an increasing number of cells will vibrate to that frequency. Consequently. the brain will perform in that mode, such as beta which promotes alertness. Gamma frequencies are often deficient in Alzheimer’s patients, and there is animal research indicating that promoting gamma frequencies will slow the onset of AD and tau deposits (MacFarlane MP, Glenn TC, 2015).
Intensity. Magnetic field intensity (flux density) is basically a measurement of the strength of a magnetic field. The intensity of a magnetic field is responsible for how much charge is induced in the stimulated tissues. The intensity is often defined by the power of the device. By varying degrees, that determines the strength of the magnetic field, and therefore the amount of stimulation that accompanies it.
Medical PEMF. Devices are available that are more powerful than the ELF PEMF designed for home use. Higher-intensity devices are available for use by clinicians that range from 200 gauss to 8,000 gauss. A device that I would use in clinical practice for brain treatment would be 2,000 gauss ($4,600), or a 4,000 gauss unit ($6,000 – $7,000). A device that enables treatment of two areas of the body at the same time runs approximately $13,000. As the intensity deliverable by the machine increases, the price typically increases. Often practitioners can manage to provide substantial treatment using moderate intensity devices.
Duration. For low intensity systems, intensity is not a concern. If I am treating a patient with exquisite sensitivity, I go “low and slow.” In clinical practice, the provider becomes highly familiar with their device of choice, so treatment involves getting to know the patient and their specific response to that particular device.
TREATMENT OUTCOMES
Bone and wound healing. The FDA approved pulsed EMFs (biphasic low frequency signal) for the treatment of fractures with delayed bone healing in 1979. (Andrew, Bassett, Pawluk, Pilla, 1974; Bassett, Pawluk, Pilla, 1974; Bassett, 1993). Beneficial effects on wound healing have been documented for three decades. A study published in 1992, for example, reported: “Wound surface area, ulcer depth, and pain intensity were assessed at weeks 0, 4 and 8. At week 8 the active group had a 47.7% decrease in wound surface area vs. a 42.3% increase for placebo (P < 0.0002)” (Stiller, Pak, Shupack, et al., 1992).
Nerve regeneration. Animal research has been conducted over the past three decades. It has found evidence that PEMF can support regeneration of nerve tissue. (Rusovan & Kanje 1991; Rusovan, Kanje, & Mild, 1992; Bervar, 2005; Das, Kumar, Jain, Avelev, & Mathur, 2012; Susynski, Marcol, & Szajkowski, et al. 2014; Stölting, Haralampieva, Handschin, Sulser, Eberli, 2016; and Ross, Syed, Smith, & Harrison, 2017). We see this in patients with neuropathic numbness who begin to experience paresthesias once the nerves begin to recover.
Sleep issues. In a double-blind study using a 4 Hz (5 gauss) unit, researchers found that this intensity and frequency were effective in reducing sleep disturbances within six weeks in 83% of the treatment group, compared with 57% in the controls. Another study, a four-week double-blind, placebo-controlled clinical trial, involved 100 people with insomnia (sleep latency, interrupted sleep, or nightmares). Some 90% of the treatment group experienced clear or substantial improvement, whereas approximately 50% of the placebo group benefitted. (Pelka, Jaenicke, Gruenwald, 2001).
NEUROCHEMICAL DISORDERS
Bipolar disorder and depression. PEMF therapy was found to produce rapid mood elevation in depressed patients with bipolar disorder (Rohan, Yamamoto, & Ravich, 2014), as well as other depressive disorders (Leuchter, Cook, Jin, & Phillips, 2013). Another study found that after five weeks of active treatment with low-intensity transcranial PEMF (T-PEMF), there was a 62% reduction on a Depression Rating Scale among those in the active T-PEMF group (Martiny, et al., 2010).
This study also found that improvement was noticeable within the first weeks of therapy. A home study of patients with depression using the T-PEMF reported that progress was gradual but sustained. At five weeks, only 27% had obtained relief. However, after eight weeks of daily treatment, 73% of subjects were relieved of their depression. Two years after the treatment, 52% of subjects were still in remission, and those who were not in remission, found relief after another course of treatment (Bech, Lindberg, Strasso, et al., 2015; Strasso, Lauritzen, Lunde, et al., 2014).
NEUROLOGICAL PATHOLOGY
Mechanisms of action. Consequentially, in PEMF studies conducted on nerve tissue cells in the laboratory setting, preliminary data suggest that exposure to a PEMF of short duration may have implications for the treatment of acute stroke. PEMF exposure counteracted low oxygen supply (hypoxia) damage significantly, reducing cell death by inhibiting activation of various tissue chemical processes involved in oxygen deprivation. Furthermore, PEMFs significantly decreased low oxygen-induced oxidative stress after 24 to 48 hours. Moreover, PEMFs were able to reduce some of the most well-known inflammatory cytokines, including TNF-α, IL-1ß, IL-6, and IL-8 (Vincenzi, Ravani, Pasquini, et al., 2016).
Memory loss. Moreover, Studies have been performed over the past 25 years to investigate the effects of low-intensity PEMF stimulation on memory processing and attention (Başa, Schürmann, Başar-Eroglu, & Karakaş, 1997). Researchers at Northwestern University studied the use of PEMFs to stimulate the brain in older adults to determine whether they could improve memory by stimulating the parietal lobe. Stimulation was performed using a 100 gauss PEMF at 10 pulses per second for 20 minutes in each session, over five consecutive daily sessions. Full intensity stimulation was compared to low intensity “sham” stimulation.
Furthermore, the researchers also used functional MRI (fMRI) to check brain function and neurological activity between the parietal lobe and the hippocampus. By the completion of the study, the memory tasks of the older individuals had improved so much that they now appeared similar to the younger control group. Therefore, memory loss was reverse-aged with active PEMF stimulation (Nilakantan, Mesulam, Weintraub, et al., 2019).
Multiple sclerosis. Additionally, a study of relapsing remitting multiple sclerosis comorbid with TBI reported that no patient showed evidence of relapse during the follow-up of at least 8 months. The authors concluded that magnetic brain stimulation was easy to perform, painless, and safe. (Ingram, Thompson, & Swash, 1988).
Inflammation. Conversely, the longer inflammation persists after even a mild neurological injury, the more damage is done to nerve tissues, which may become ultimately unrecoverable. In this context, an animal study of TBI explored whether PEMF signals could alter the course of inflammation. Cytokine IL-1ß levels in cerebrospinal fluid (CSF) were proportional to injury severity in brain bruise injury. PEMF treatment applied continuously reduced IL-1ß levels by up to ten-fold in CSF within six hours after injury, and significantly suppressed IL-1ß within 17 to 24 hours after injury (Rasouli, Lekharaj, White, et al., 2011).
Ischemia, ten minutes post-blockage. On the other hand, In an animal study involving blockage of the carotid artery, PEMF treatment at 75 Hz was initiated ten minutes after onset of ischemia and continued throughout the recovery of the blood supply. The PEMF did not reduce the total area of injury evident on MRI. However, PEMF reduced brain edema by 65%. Subsequently, the PEMF-treated group evidenced double the recovery, 55% vs. 28% (Grant, Cadossi, Steinberg, 1994).
Post-stroke, three to four weeks previous. Simultaneously, forty-eight patients (average age 45-48 years old) three to four weeks post-stroke were divided into two groups and provided with the same rehabilitation program. Patients in the treatment group were additionally exposed to a standard series of 10 ELF-EMF treatments, for 15 mins at 5 mT (50 gauss), 40 Hz. The PEMF group had double the amount of BDNF (brain-derived neurotrophic factor), 50% increases in VEGF (vascular endothelial growth factor), and 2.5 times more gene expression. Clinically, the PEMF group averaged 35% better cognitive functioning and 45% better depression scores. In the non-PEMF group, stroke scale severity and function measures were typically 65% and 50% worse, respectively (Cichoń, Bijak, Czarny, et al., 2018).
Post-stroke, six months previous. A study of higher-intensity, low-frequency TMS PEMF for stroke investigated the long-term behavioral and neurophysiologic effects of combined HI-PEMF and physical therapy (PT) in chronic stroke patients with mild motor disabilities more than six months post stroke. In this study, 30 patients were enrolled in a double blind, randomized, single-center clinical trial. Patients received two PEMF sessions per day, 25 minutes each, 1 Hz high-intensity PEMF over the intact (not affected) motor cortex with standard task-oriented upper limb exercise PT. The real treatment group had greater behavioral and neurophysiologic improvements, particularly in the group receiving treatment before PT, with robust and stable improvements (Avenanti, Coccia, Ladavas, et al., 2012).
Post-stroke, two to twenty-four months previous. Likewise, In a lower intensity PEMF study, 95 patients with spastic paralysis received treatment three times per day using 40 Hz, 10 mT (100 gauss), for 12 minutes, over 21 days, and repeated every six to eight weeks. Patients also received medication and physical therapy. Improvements in actively treated patients included significant decrease of muscle tension (88%), increased muscle contraction force (76%), increased active motion of paralyzed limbs (74%), improved gait (71%), and decreased aphasia (64%) (Sieron, Cieslar, Adamek, et al., 1996).
Post-stroke, one to ten years previous. Another study of stroke rehabilitation using low-frequency PEMF treated patients who had incurred a stroke years earlier (within the past 10 years). During a 15-day rehab hospitalization, each person received 22 treatment sessions of 20-minute low-frequency PEMF and 120-minute intensive occupational therapy (OT) daily. The PEMF of 1 Hz was applied to the side of the head opposite the area of the stroke, i.e., on the same side as the paralysis. Improvements were seen up to four weeks after discharge in 39% of patients. Researchers concluded that a 15-day inpatient PEMF treatment plus OT protocol is clinically useful neuro-rehabilitation for post-stroke patients with upper limb paralysis (Kakuda, Abo, Shimizu, 2012).
TBI Study. A pilot study was recently completed with a group of ten individuals with a history of concussion/TBI. In some cases, the injuries were more than ten years old. Using a medium intensity 10 Hz PEMF device applied to the head (front to back or side to side), patients were treated for two hours a day for three months. Everyone in the study noticed benefits. An objective measure of brain function was used to gather information before and after treatment and showed clear improvements over baseline scores, as well as important clinical improvements and better cognitive focus (Pawluk, 2019) Also note that research has reported improvement in post-concussion headaches treated with PEMF for as little as 30 minutes (Grunner, 1985).
In situations involving neurological insult such as a stroke, treatment with a PEMF device for even short durations may have positive implications for recovery and for the treatment of acute stroke. While it is difficult for the medical system to be able to treat people in the acute phase of brain injury, whether it is stroke or trauma, if an individual owns a PEMF system, that can be used immediately and continually to reduce the extent of the damage. This is critical in improving the prognosis and in reducing the length of time for more complete recovery.
William Pawluk, MD, MSc
Dr. William Pawluk is a holistic physician located in Townsend, MD in the Baltimore metropolitan area, with past appointments at Johns Hopkins University and the University of Maryland. With a background in family medicine, he has additional training in functional medicine, nutrition, acupuncture, homeopathy, hypnotherapy, bodywork, and energy medicine. He is the foremost authority on Pulsed Electromagnetic Field therapy in North America, with 30 years of experience in clinical applications of PEMF for healing, regeneration, and holistic pain management.
Author of Power Tools for Health, a comprehensive book on the research and usage of PEMFs in healing, he has also written professional book chapters and numerous journal articles. and provided more than 50 interviews for radio, podcasts, magazines, and TV. He has been cohost of a two-hour holistic health radio show for the past ten years and host of the Pain Solution Summit, www.painsolutionsummit.com. In 2019, Dr. Pawluk received the ACIM Lifetime Achievement Award for work with Magnetic Field Therapy.
William Pawluk, MD, PC
1001 Cromwell Bridge Rd., #312, Towson, MD 21286
866-455-7688
www.drpawluk.com
PEMF Devices. Dr. Pawluk has purchased, tested, and validated approximately 100 different PEMF devices over the 30 years he has worked in this field. Based on his experience, a number of devices are recommended and available for purchase on his website, drpawluk.com. They include: local and whole-body systems, both battery and AC-powered devices, intensities of devices range from very low intensity (<1 Gauss), medium intensity (10 – 1000) Gauss, to high intensity (2000-8000 Gauss) including devices that are able to cause muscle contractions.
Consulting services. Dr. Pawluk provides consulting services to both consumers and practitioners. Consultations are recommended for practitioners to be able to have more certainty about the most appropriate tools for the professional setting. Many professionals spend much more than they need to for PEMF systems. On the other hand, many professionals also acquire PEMF systems that are not likely to provide much benefit quickly in the practice setting.
Website. drpawluk.com is an extensive resource for patients, with basic educational information, more than 40 blogs with references, numerous videos, and a virtual store from which devices may be purchased. Once devices are purchased Dr. Pawluk and his staff provide significant ongoing support for both initial use and subsequent informational needs.
Book. Power Tools for Health is a readable, highly referenced work on basic concepts in the application of PEMFs. These include mechanisms of action, an extensive clinical section on 50 different health conditions, and more than 500 references on laboratory findings and clinical trials.
REFERENCES
Andrew C, Bassett L, Pawluk RJ, Pilla AA. Augmentation of bone repair by inductively coupled electromagnetic fields. Science (80-). 1974;184(4136):575–577. doi:10.1126/science.184.4136.575
Avenanti A, Coccia M, Ladavas E, Provinciali L, Ceravolo MG. Low-frequency rTMS promotes use-dependent motor plasticity in chronic stroke: A randomized trial. Neurology. 2012 Jan 24;78(4):256-64.
Başar E, Schürmann M, Başar-Eroglu C, Karakaş S. Alpha oscillations in brain functioning: an integrative theory. Int J Psychophysiol. 1997 Jun;26(1-3):5-29.
Bassett CAL. Beneficial effects of electromagnetic fields. J Cell Biochem. 1993;51(4):387–393. doi:10.1002/jcb.2400510402
Bassett CAL, Pawluk RJ, Pilla AA. Acceleration of fracture repair by electromagnetic fields. A surgically noninvasive method. Ann NY Acad Sci. 1974;238(1):242–262. doi:10.1111/j.1749-6632.1974.tb26794.x
Cichoń N, Bijak M, Czarny P, et al. Increase in blood levels of growth factors involved in the neuroplasticity process by using an extremely low frequency electromagnetic field in post-stroke patients. Front Aging Neurosci. 2018 Sep 26;10:294.
Cichoń N, Czarny P, Bijak M, et al. Benign effect of extremely low-frequency electromagnetic field on brain plasticity assessed by nitric oxide metabolism during poststroke rehabilitation. Hindawi. 2017;ID 2181942:9. | https://doi.org/10.1155/2017/2181942
Grunner O. Cerebral use of a pulsating magnetic field in neuropsychiatry patients with long-term headache. EEG EMG Z Elektroenzephalogr Verwandte Geb (1985) Dec;16(4):227-230.
Iaccarino HF, Singer AC, Martorell AJ, et al. Gamma frequency entrainment attenuates amyloid load and modifies microglia. Nature. 2016;540:230.
Ingram DA, Thompson AJ, Swash M. Central motor conduction in multiple sclerosis: evaluation of abnormalities revealed by transcutaneous magnetic stimulation of the brain. J Neurol Neurosurg Psychiatry 51(4):487-494, 1988.
Kakuda W, Abo M, Shimizu M, et al. A multi-center study on low-frequency PEMF combined with intensive occupational therapy for upper limb hemiparesis in post-stroke patients. J Neuroeng Rehabil. 2012 Jan 20;9(1):4.
Leuchter AF, Cook IA, Jin Y, Phillips B. The relationship between brain oscillatory activity and therapeutic effectiveness of transcranial magnetic stimulation in the treatment of major depressive disorder. Front Hum Neurosci. 2013 Feb 26;7:37.
Nilakantan AS, Mesulam MM, Weintraub S, Karp EL, VanHaerents S, Voss JL. Network-targeted stimulation engages neurobehavioral hallmarks of age-related memory decline. Neurology. 2019 May 14;92(20):e2349-e2354.
Pawluk, W. The role of pulsed magnetic fields in the management of concussion and traumatic brain injury. J Science and Medicine, 2019(1):1-12.
Rohan ML, Yamamoto RT, Ravichandran CT, et al. Rapid mood-elevating effects of low field magnetic stimulation in depression. Biol Psychiatry. 2014 Aug 1;76(3):186-93.