Reduce Pain During and After Shingles
Table of Contents

The pain associated with shingles (herpes zoster – HZ) is one of the most intolerable pains people have to endure. And, about 1 out of 5 people, after a shingles attack, will experience a worse, persisting, and debilitating pain called postherpetic neuralgia (PHN). The pain can get better after a few months, though in some people it will last even longer. Doctors don’t know why shingles converts into PHN. PHN is considered neuropathic pain or a form of neuropathy.
SHINGLES ATTACKS – SYMPTOMS, REACTIONS AND PAIN
One million shingles attacks occur every year in the US, and one in every three people develops shingles during their lifetime. The shingles virus (called the varicella zoster virus or VZV) is the same virus as the chickenpox virus. The first infection with the virus (the primary infection) is chickenpox, typically occurring in children. Shingles (a secondary condition) is a consequence of the first infection, chickenpox. Prior to the use of childhood vaccines in the U.S., more than 90% of Americans had chickenpox before the age of 20. After a chickenpox infection heals and immunity develops, the virus becomes dormant, and lives and persists in a cluster of nerve cells (a ganglion) in a spinal nerve anywhere along the spine.
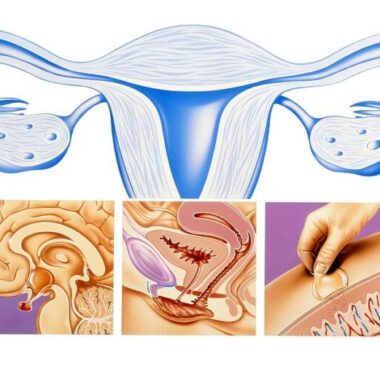
A shingles outbreak develops when the dormant chickenpox virus is reactivated in the spinal nerve roots, then migrates to the nearby related sensory nerves, causing a rash along that sensory nerve’s pattern (dermatome). Most commonly the rashes occur on either the head, face, chest or torso. The course of shingles and pain is usually one-sided and follows the affected sensory nerve pattern (dermatome) on that side. Because the dormant virus is normally suppressed by the immune system, reactivation only occurs in people whose immunity is weakened, whether temporarily, or as a factor of age. Psychological stress, or a dramatic life event may contribute to shingles flare-ups. People can have multiple shingles attacks in a lifetime.
POSTHERPETIC NEURALGIA (PHN) – WHAT YOU NEED TO KNOW
20% of people aged 60–65 years will develop PHN, and more than 30% of those over 80 years will develop it. In addition to age, risk factors for developing PHN after shingles are based on the way the shingles attack shows itself:
- pain or abnormal sensations before the rash shows up,
- severe rash (that is, more than 50 skin lesions or blisters,
- severe pain during the acute attack.
By way of example, an elderly woman with severe pain and a sudden onset rash has a greater than 50% chance of developing PHN, whereas her risk is only 10% when none of these factors is present.
In the first stages of the shingles attack, pain is typically moderate to severe. Those suffering from a shingles attack have ranked the pain as more intense than post-surgery, or labor pains. However, PHN can develop into chronic pain, which can seriously affect a person’s ability to continue regular activities. This pain can become relentless and can persist for months or even years after the acute disease phase. In one study of people over 65 years old with PHN, the average length of pain was 3 years, and ranged from 3 months to more than 10 years.
Those with PHN experience three major types of pain, lasting for at least 3 months after healing of the skin rash caused by shingles:
1) constant burning, aching, or throbbing pain,
2) intermittent stabbing, shooting, or electric shock-like pain, that can happen without a stimulus, and
3) pain brought on by a stimulus, such as a light touch, but not proportional to the stimulus (exaggerated pain).
Additionally, those with PHN have reported other abnormal sensations in the skin. These have been described as itchy, burning, restrictive, numbness or feelings of pins-and-needles. Those with PHN have reported a severely decreased quality of life due to interference with daily activities and functions, decrease in physical ability, and the psychological toll it can take. As a result, PHN is usually accompanied by anxiety, depression, and dissatisfaction or frustration in being able to fulfill hopes or expectations.
TREATMENT OF PHN
Shingles attacks are frequently treated with antiviral medications. These medications do not kill the virus, but instead limit its growth so that the attack may be less severe. A more effective strategy may be to get shingles immunizations; though even these do not prevent future shingles attacks, but may limit the likelihood or degree of PHN. In other words, they are not foolproof.
Once it develops, there is no cure for PHN. Controlling pain is the primary treatment strategy. Medication and nerve destruction are the most common therapies in medical practice. Pregabalin and gabapentin, the two most widely used drugs, are often only slightly helpful. A survey conducted in 2002 of 385 patients aged 65 years or older with persistent PHN who were receiving prescription medication, found that only 14% were highly satisfied with their treatment (Bonezzi). Although these therapies can partially relieve the pain, they may cause undesirable side effects and high risks of complications. Therefore, therapies that can relieve neuropathic pain safely and noninvasively without causing severe side effects are desperately needed.
PULSED MAGNETIC FIELD DEVICE (PEMF) THERAPY RESEARCH FOR TREATMENT OF PAIN RELATED TO SHINGLES AND PHN
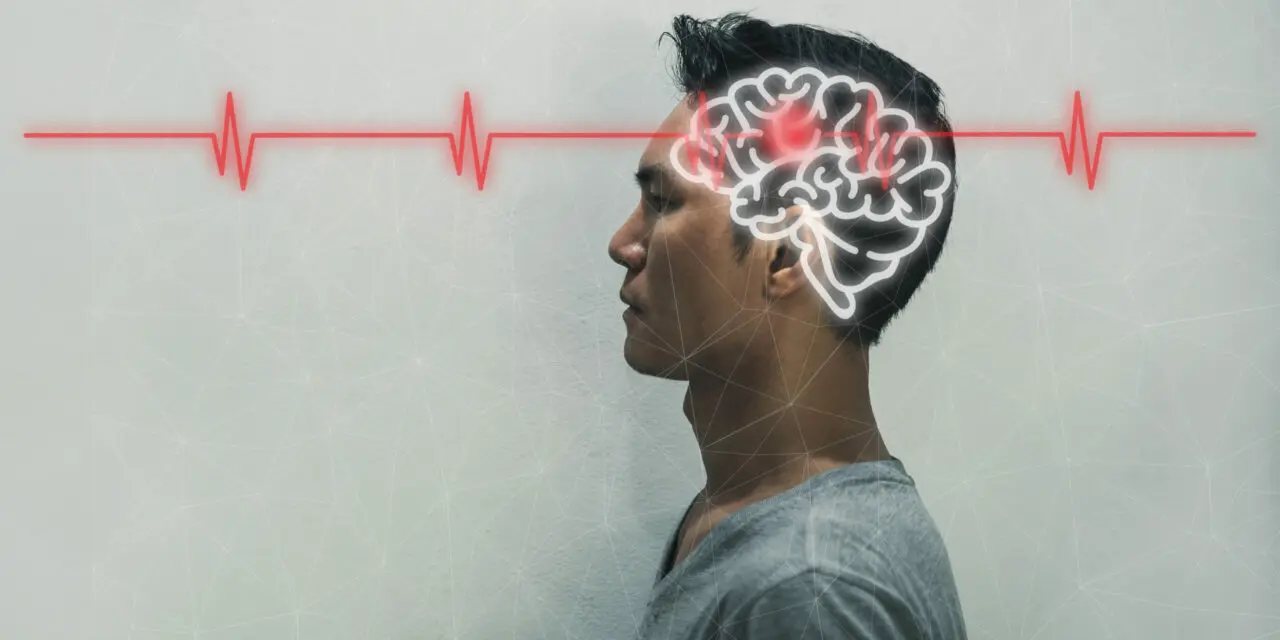
Pulsed magnetic field device (PEMF) therapy was recently studied to see if it would be beneficial to those suffering with PHN. PEMF device therapy is painless and noninvasive. Because PEMFs cross through the brain, the form of PEMF therapy used in the study was applied to the skull; this is called transcranial magnetic stimulation (TMS). TMS has a painkilling analgesic effect level similar to a surgically placed, epidural electrical stimulation implant. It is dissimilar, however, to the electrical stimulation implants, in that TMS does not have a high risk of failure and complications. Additionally, TMS device-type magnetic fields can also be used to stimulate peripheral nerves and muscles.
Because it is painless and noninvasive, TMS is considered one of the most important brain technologies of the 21st century. TMS is being widely applied in clinical psychiatry, for neurologic disorders, and in rehabilitation. Studies have proven that TMS is effective in improving pain, sleep quality, and anxiety of patients with PHN.
One study (Pei) evaluated the use of TMS for PHN. In this study, 3 treatment schemes were used, equipment placed over the head but not actively stimulated (sham), TMS at 5 pulses per second [PPS], and 10 PPS. The effectiveness and safety of these treatments were compared to see which treatment scheme might be best.
Methods: Sixty patients with PHN were divided into 3 equal groups. TMS was applied with a coil to the side of the head just above and behind the ear (over the primary motor cortex – M1) on the healthy side of the body. Active stimulation was at an intensity of 80%, once daily for 10 days. For the 5-PPS group, each session included 300 one-second pulses at 5 PPS for a total of 1500 pulses per session.
For the 10-PPS group, each session had 300, 0.5-second pulses, for 1500 pulses per session. In all groups, total session time was 17.5 minutes. All had conventional medication therapy. Everyone received evaluations at different time points (before treatment (T0); 10 times during treatment (T1-T10); 1 month after treatment (T11); and 3 months after treatment (T12). Evaluations were for level of pain (VAS), quality of life (QOL), sleep quality (SQ), depression (SDS), and impression of change (PGIC), and incidence of adverse events.
Results: Compared with the sham TMS group, there was a significant reduction in pain scores in the active treatment groups at T2-T12. Pain scores in the 10 PPS TMS group at T7-T12 were significantly better than the 5 PPS group. The average pain score reduction was 28% with 5 PPS TMS compared to 40% with 10 PPS TMS. The quality of life, sleep and impression of change scores of both the active treatment groups at 3 months (T12) after the treatments ended were significantly better than the sham group. This indicated that there were long-term benefits from PEMF device TMS treatment, including in quality of life and sleep quality.
Pain score reduction in the 5 PPS group was not as good as the 10 PPS group. The same was true for quality of life and sleep scores. This is presumed to be because 10 PPS may be more alerting to the brain through the entrainment effect of more rapid, alpha frequency pulses.
As is usual with PEMF studies, adverse events among the 3 groups after TMS were not significant.
OTHER RESEARCH INTO PEMF THERAPY FOR PAIN
Other research (Ma) also found that PEMF device treatment with TMS was safe and effective. Mean pain scale (VAS) reduction in the real TMS group was 17% for people who had PHN longer than 6 months. VAS was significantly reduced by 100% compared to sham for the real TMS group along the whole time-course of the study. No significant daily pain level changes were seen for sham TMS. For those whose pain scores before starting PEMF device TMS treatment were greater than 7 of 10, the reduction in pain was 52% compared to a 30% reduction in those whose scores were less than 7. These pain reduction and analgesic benefits were followed by long-term improvement in quality of life. Reduction in need for medications at week 5 was significantly better in the active TMS magnetic device group than in the sham group.
In the real PEMF device TMS treatment group, six patients reported minor adverse events with four reports of neck pain and headache, and two reports of dizziness and dry mouth. These did not require a change in treatment. Of the 20 patients from the sham TMS group, four also complained of neck pain and headache, and one complained of dizziness. Essentially there was no difference. So, it’s unlikely that TMS treatment was the cause of the symptoms.
SUMMARY
It may seem counterintuitive to treat the brain for chronic pain, whatever the cause, when the pain is caused by a problem, or felt elsewhere in the body. Too often, people treat where they feel the pain but not the source of the pain. Treating the actual area of the pain, where the blisters were, is less likely to produce significant benefits.
The source of the pain in PHN is coming from the nerve roots at the level of the spine from which the shingles pain signal starts. At the very least treatment needs to be to the spine at the level where the nerves are affected. These two brain PEMF device stimulation studies seem to indicate a major improvement in pain. However, sleep, and quality of life in people with chronic, long-lasting PHN, these benefits were not from treating the specific areas generating the pain or the areas where the pain was felt.
This brain transcranial magnetic stimulation (TMS) research used a different approach. It recognized the need to treat the brain itself, which is the “last stop of the train” of the pain signal.
PHN is commonly severe, disabling, and potentially very chronic. I normally recommend using higher intensity PEMF device treatments to deal with this type of pain. Based on the TMS research, magnetic field intensities needed to treat the brain adequately are over 5000 Gauss [500 mT]. It’s possible that lower magnetic field intensities may be useful to treat the nerve roots. More information about the level of the magnetic field needed to treat the cause of the pain, that is, inflammation, can be found here.
For the most dramatic PEMF device PHN pain-reducing results, I would recommend a combined 3 level approach.
- treat the area where the pain is felt,
- treat the spinal cord level where the pain is generated, and
- lastly, treat the brain, which is dramatically affected by the pain to cause “chronic pain brain.”
It would be best to have a PEMF system with at least 2000 gauss and preferably closer to 4000 Gauss. These intensities are still less than the scientifically studied PEMF device TMS systems. These are around or above 5000 Gauss.
The other important thing to consider is that PHN can be chronic and will likely require ongoing treatments. The length of time treatments will be needed is entirely individual. In both the studies I mentioned above, people received daily treatment for 10 days. Even though pain was reduced by 28-40%, it was not relieved completely. It is not known yet whether treatment beyond 10 days would produce even better results. My clinical experience is that longer courses of treatment are needed for the best results.
Also, the Pei study showed that pain continued to decrease from a level of 6.3 out of 10 to 4.3. This was true as long as treatment continued over the 10 days. Even at that lowest level (4.3), that is still a significant amount of pain, and would dramatically affect the quality of life. The goal should be to try to reduce the pain to 0 if possible.
Another consideration is that this research was limited to people who already had established (PHN) and was not done at the time of the initial shingles attack. The sooner treatment begins after a shingles attack starts, the better and more long-term the results will be. Ideally, treatment should begin at the first sign of shingles. This will not only help to reduce the pain of the shingles during an attack, but will also help to reduce the likelihood of the shingles developing into PHN.
If a person waits to start PEMF device treatment after PHN has developed, it will be much more difficult to reverse the problem. The longer treatment is delayed after shingles starts, the more the nerve inflammation and infection can progress. This leads to more and more nerve damage (neuropathy) and pain. Unfortunately, antiviral medications do not kill the viruses that cause shingles and PHN. All they do is to stop the virus from reproducing even more. Nevertheless, they are still useful. And pain medications do nothing to stop the progression of the damage. They don’t limit the attack and will not reverse it or reverse the nerve damage. In fact, some research shows that pain medications may significantly inhibit natural anti-viral white cells. These are called natural killer (NK) cells, which attack and destroy viruses.
So, it makes a lot of sense to combine PEMF device treatments with antivirals and NK cell activator supplements. This controls the shingles and subsequent PHN.
PEMF FOR SHINGLES AND PHN – THE BOTTOM LINE
PEMF device therapy can be extraordinarily useful with shingles attacks. They can be used used until after postherpetic neuralgia (PHN) starts. They can still be very helpful to decrease pain levels and improve quality of life. Getting and using the right intensity magnetic field becomes critical to getting the right level of benefit. Following a 3 level PEMF device treatment approach should give the best results for this serious and disabling PHN condition.
REFERENCES
- Bonezzi C, Demartini L. Treatment options in postherpetic neuralgia. Acta Neurol Scand. 1999;100:25–35.
- Ma SM, Ni JX, MD, Li XY, et al. High-Frequency Repetitive Transcranial Magnetic Stimulation Reduces Pain in Postherpetic Neuralgia. Pain Medicine 2015; 16: 2162–2170.
- Mallick-Searle T, Snodgrass B, Brant JM. Postherpetic neuralgia: epidemiology, pathophysiology, and pain management pharmacology. J Multidiscip Healthc. 2016 Sep 21;9:447-454.
- Pei Q, Wu B, Tang Y, et al. Repetitive Transcranial Magnetic Stimulation at Different Frequencies for Postherpetic Neuralgia: A Double-Blind, Sham-Controlled, Randomized Trial. Pain Physician. 2019 Jul;22(4):E303-E313.