Urinary Incontinence and OAB
Table of Contents

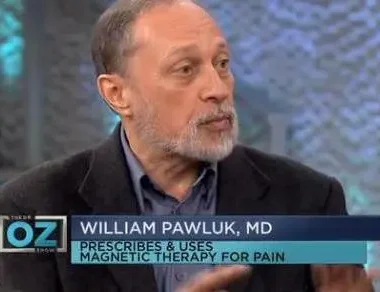
I have been a family physician for more than 40 years. I have helped hundreds of women with life-limiting and embarrassing incontinence and OAB issues. Most of the time, treatment was frustrating and only partially successful. I have always looked for alternative approaches that were not invasive to help with this condition. Even these did not often work successfully.
I have worked with PEMFs for a vast range of health issues for a long time. I have encountered interesting responses from patients, particularly females, who have had improvements in their urinary incontinence issues from the use of PEMFs.
THERE ARE STUDIES SUPPORTING PEMFS FOR URINARY INCONTINENCE
Because of these observations, I decided to do a review of the scientific literature on the use of PEMFs for this problem. I was pleasantly surprised to see a reasonably significant number of articles describing research being done on urinary incontinence and overactive bladder. This research is very promising and ranges from the use of high intensity PEMF systems in the professional office setting to the use of much lower intensity PEMF systems in the home setting. My experience has been that high intensity PEMF systems can often get good results in a short time, but often the results don’t last.
This is because high-intensity PEMF systems do not always create a physical change in the tissue in the short time in which they are used. This means that they will require multiple courses of treatment over the years. On the other hand, using a home-based, battery-operated PEMF system, worn over the bladder area, many hours a day, possibly even overnight, seems to be very effective, and possibly over the long run even more effective. This is true because of the need to change the physical characteristics of the bladder itself in terms of the inflammation, bladder muscle irritability, and reduce the number of overactive nerve cells contributing to the problem. PEMFs lend themselves extraordinarily well to this complex set of changes that happen in the bladder over time to create an overactive bladder, leading to incontinence.
Better solutions than the current medical solutions (typically medications, procedures or surgeries) are necessary. Electrical stimulation, as noted in a recent study, is not anywhere as effective as PEMF therapy (and nowhere near as comfortable). But, electrostimulation is in the domain of the practitioner and healthcare facility, and that is what they are going to recommend, because that is the only tool they have. We know now as well that pelvic exercises don’t work over time.
Certainly pelvic exercises do make any kind of other external stimulation approach work even better. Many women begin to actually recognize contractions of their pelvic muscles after using high-intensity PEMFs. Then, they can go home with a home-based PEMF stimulation system to finish the job. But, using high-intensity PEMFs to begin a course of treatment is not necessary, since home-based PEMF systems will work well over time anyway, and Kegel exercises may not be necessary.
In my review of the science, it’s clear that high intensity PEMFs do improve OAB and urinary incontinence significantly, including positively changing the underlying causes of the incontinence in the bladder tissue itself. At the same time, research is showing that even very low intensity magnetic fields, worn throughout the day for upwards of 2 months at a time also produce improvement. Some of the studies at the lower intensities used 10 Hz and 18.5 Hz, both producing positive results.
Higher intensity systems are typically limited to much lower frequencies, or repetition rates, usually less than 10 Hz. But from all of this research, there is still no certainty as to which frequency or intensity works best. From my experience, it’s probably much more important to be using PEMF therapies of whatever kind, on a consistent basis, over the bladder or pelvic area, daily, for an extended period of time. In the long run, this is going to create the physical changes in the bladder that are necessary to reverse the tissue changes causing the bladder overactivity problem. The body has its own pace of healing and we need to acknowledge and respect that.
So, from this review I’m optimistic that we can offer significant relief to millions of women suffering from overactive bladder and urinary incontinence unnecessarily, given the inexpensive, comfortable home-based PEMF solutions available. These are expected to produce much better long-term results than current therapies, with a lot less risk.
As an aside, while most of this review is focused on female urinary incontinence, a number of the studies within included males in their research. Males often had similar results to females in the improvement of their OAB and urinary incontinence. So, ladies, if you have male partners, family members or friends who suffer from incontinence, this technology are likely to benefit them as well.
Over the years of practicing medicine, I have worked with hundreds of women with urinary incontinence. Most of the time these were women who had delivered babies. It’s commonly accepted that women who delivered babies naturally would be expected to have stress urinary incontinence down the road. That was the old thinking. It made sense at the time. However, as we have learned more and more about this common and very stressful problem, we have discovered that it is not as simple as the stretching of the tissues of the birth canal with the birth process.
We were all taught that women needed to do pelvic exercises to strengthen the muscles of the pelvis [Kegel exercises] to reduce the symptoms of stress incontinence. Again, that was a very simplistic approach in hindsight. A whole new concept of what is going on with urinary incontinence (UI) has emerged as science has evolved.
URINARY INCONTINENCE: WHO IS AFFECTED?
At minimum, 11 to 16 million women in the United States cope on a daily basis with symptoms that include sudden strong urges to urinate, difficulty delaying urges to urinate, frequent trips to the bathroom, and in many cases involuntary loss of urine when urgency strikes. They may wear pads or adult diapers for accidents, plan ahead for access to bathrooms, and modify their social and work lives to accommodate their symptoms. Some are very distressed by the symptoms, whether mild or severe, and others find mechanisms to adapt, reporting little trouble with symptoms or interference with normal routines.
Others report their symptoms negatively influence quality of life factors, including: loss of self-esteem, attractiveness, and sexual function. The majority of women believe that some amount of urinary incontinence is inevitable with aging. Women with these symptoms tend to not talk with their health care providers concerning their bladder dysfunction, and providers may not routinely inquire. As a result, a small minority receive treatment.
Between 10-40% of women have UI (possibly even more), and the percentage increases with age. There are 3 basic types of UI: stress, urge, and mixed. Overall, about half have stress incontinence, a smaller proportion have mixed, and the smallest is urge. Since women often have mixed incontinence [MI], the more commonly used term today is overactive bladder [OAB]. OAB with urge incontinence happens in 10% of women 18+ years of age (less than 5% in the age group 18–44 and up to 19% in the 65+ age group).
The severity of the symptoms is critical to determining treatment approaches and the likelihood of success of treatment, and severity increases with age. Significant incontinence is present in 9-13% of women over 55. Remission or improvement in UI is seen particularly in stress incontinence and primarily because women develop coping strategies that decrease the reported frequency of episodes of UI. Not so with OAB, which typically can get worse with time or age.
TRADITIONAL TREATMENTS: OUTCOMES AND COSTS
Urinary incontinence is an important health problem to the individual sufferer and to health services. Risk factors for UI include age, pregnancy and childbirth, menopause, hysterectomy, obesity, lower urinary tract symptoms, functional or cognitive impairment, occupational risks, family history, genetics, and a host of other factors, including diabetes, use of diuretics, cigarette smoking, dementia, etc.
Treatments include prescription medications or patches, surgeries and procedures (including sacral neuromodulation and botulinum injections), behavioral interventions such as bladder training, and complementary and alternative medicine options such as acupuncture and reflexology.
All these treatments, of course, have varying success rates.
DRUG TREATMENT
All drug treatments are effective at improving one or more overactive bladder [OAB] symptoms when compared to placebo. Reductions ranged from 0.9 to 4.6 incontinence episodes per day across all drug treatments and from 0.7 to 4.2 in voids per day. No one drug is clearly better than others. Extended release formulations taken once a day reduce urge urinary incontinence [UUI] by about 2 episodes per day, and total urinations by 2 per day. Immediate release forms taken twice or more a day reduce UUI episodes by 1 per day, and urinations by 2 per day. Of note, placebo reduces UUI by 1 and voids by 1 per day. Even with these small results on symptoms, drug treatments increase quality of life and reduce distress, compared to no treatment.
SURGICAL TREATMENT
Procedures and surgical treatments include sacral or peripheral neuromodulation, bladder instillation or injection of drugs, bladder distention, and cutting nerves to the bladder. The strength of the evidence for managing OAB with procedural and surgical treatment is weak outcomes of this care.
Stress incontinence is more often managed by surgery due to advances in surgical techniques. While not well proven for its value, most clinicians use invasive urodynamic testing (IUT) to prove stress incontinence before offering surgery. IUT is expensive, embarrassing and uncomfortable for women.
BEHAVIORAL TREATMENT
Behavioral interventions include bladder training and more complicated behavioral training (with or without biofeedback), pelvic muscle exercises, vaginal electrical stimulation, and caffeine reduction. Managing OAB with behavioral treatment approaches alone gets moderate to weak short term benefits and weak benefits in the long term. Still, overall, behavioral approaches can reduce episodes of incontinence and daily voids at least somewhat. Complex approaches are close to drug treatment in getting modest improvements, reducing leakages by up to 1.9 per day, and emptying’s per day up to about four. Behavioral approaches do not enhance drug therapy for reducing episodes of incontinence or voiding.
COMPLEMENTARY AND ALTERNATIVE TREATMENTS
These treatment options include acupuncture, foot reflexology, and hypnotherapy. The evidence for complementary and alternative approaches to managing OAB is weak. Acupuncture may decrease frequency of voiding and symptoms of urgency, with objective evidence from bladder measurements [cystometrics]. Women felt they were improved in the bother associated with incontinence and the quality of life. The results may be similar to the use of drugs. Reflexology needs more evidence know the benefit. Hypnotherapy, or hypnosis, is likely not to be very useful. Given the big role belief plays in OAB treatment, it has been difficult to prove the value of hypnosis.
COSTS OF TREATMENTS
Total direct health care costs for women with OAB in 2000 were estimated at $6.9 billion, of which $1.1 billion were for drug treatment and $550 million for surgical treatment. Medication costs for OAB with the two most commonly used drugs ranged from $56 to $360 over a twelve month period for newly diagnosed patients. And, these drugs do not cure the problem, only control it. So, these costs will be lifetime.
The research seems to indicate that the evidence is not strong to support the current treatments for OAB. Medications can provide symptom relief which is often not complete, but suffering women see these as better than nothing, and they are convenient. Because benefits of current treatments are only modest, there is a need to consider the value of combinations of types of treatments.
One of the fundamental causes of the relatively poor performance of current treatments may well be due to a previous lack of understanding of the fundamental mechanisms involved in UI. As a result of this new information, it appears that one potentially very valuable set of tools for managing incontinence would include magnetic field therapies, particularly PEMFs.
THE LATEST SCIENCE ABOUT CAUSES
Overactive bladder syndrome (OAB) typically includes the lower urinary tract symptoms of frequency, urgency, and varying severities of urgency urinary incontinence. It is specifically defined as “urgency, with or without urge incontinence, usually with frequency and nocturia”.
NERVE GROWTH FACTOR
Other than some of the obvious causes listed above, there is now emerging a better understanding of the tissue changes involved in the bladder to produce OAB. Three hypotheses exist to explain this.
The myogenic hypothesis states that the smooth muscle cells of the overactive bladder are more susceptible to contraction, and smooth muscle bundles contract in groups, allowing for the possibility that physical changes in the muscle fibers allow local activity to spread to the rest of the bladder, making it more susceptible to spontaneous contractions.
The peripheral autonomous hypothesis states that bladder overactivity is due to enhanced coordination of muscle activity by bladder wall nerves. An imbalance of stimulation and relaxation increases autonomous activity, possibly resulting in increased bladder sensation as well as bladder overactivity.
The neurogenic hypothesis states that some nerve fibers are generally quiet during normal bladder voiding. These fibers can form new pathways, and then may be responsible for bladder pain and overactivity, carrying urinary impulses to the spinal cord.
Neurogenic theories suggest that bladder overactivity arises from generalized nerve excitation of the bladder muscle. The main trigger for changes in transmission of nerve signals from the bladder to the central nervous system may be nerve growth factor (NGF), which is elevated in OAB. Blockade of NGF by antibodies against NGF prevents frequent urination, bladder contractions, urination urge activity, and swelling of spinal cord neurons. Based on these findings, NGF plays a critical role in the pathophysiology of OAB.
INFLAMMATION
Although the cause has been divided into neurogenic and non-neurogenic types, there has also been investigation into the role of inflammation in the development of bladder overactivity.
In rats with OAB, injection of COX-2 anti-inflammatories into the bladder reduced inflammatory molecules in bladder tissue and improved bladder contraction. In experimental cystitis, treatment with a peptide that inhibits inflammatory markers reduced inflammation and nerve factors such as NGF, improving symptoms of OAB. Therefore, we can conclude that interaction among other inflammatory disorders in the body, pro-inflammatory molecules, and the peripheral and central nervous system are responsible for the development of OAB.
ALTERNATIVE TREATMENTS FOR URINARY INCONTINENCE AND OAB
At one level, anti-inflammatory drugs aid in the treatment of OAB symptoms by reducing inflammatory responses. Also, there is evidence to show that OAB may be improved by using various electromagnetic stimulation strategies.
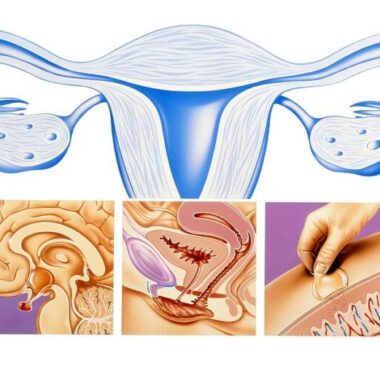
There are 3 basic approaches studied using magnetic fields to stimulate the bladder to reduce the symptoms of OAB and stress incontinence. These include static magnets, direct stimulation of the bladder, and stimulation of the nerves controlling bladder function. Stimulation of the nerves that control bladder function includes stimulation of spinal nerves, the pelvic pudendal nerve and the tibial nerve in the leg. Sacral nerve stimulation involves invasively stimulating the pelvic pudendal nerve and the sacral spinal nerve roots.
ELECTRICAL STIMULATION
Pelvic floor muscle electrical stimulation is an alternative treatment for urinary frequency and urge incontinence with a success rate from between 45% and 91%. There are various approaches for delivering electrical pulses. Use of electrical stimulation is still not commonly accepted, primarily because of discomfort and invasiveness.
Electrical sacral nerve stimulation via an implant for medication resistant OAB treatment has been studied. Sacral nerve stimulation is an increasing alternative gaining some use.
STATIC MAGNETS
With regard to the use of static magnetic stimulation of the pelvic floor, compared to placebo, the use of 15 static magnets of 800-1200 Gauss, in undergarments to the front, back, and underneath the pelvis for at least 12 hours a day for three months was studied. This study found no evidence that static magnets cure or decrease the symptoms of urinary incontinence.
MAGNETIC STIMULATION
Magnetic stimulation is a new technique for stimulating the nervous system noninvasively. It can activate deep neural structures by induced electric currents with much less or no pain.
We have mentioned many times before in other updates that a major aspect of the benefit or value of PEMFs is to reduce inflammation. In addition, there is the expectation that PEMFs should also reduce nerve cell firing (the neurogenic theory). Plus, there is evidence to show that PEMFs can also reduce muscle irritability or spasticity (the myogenic theory). Recent research showed that activating sacral bladder nerve roots by magnetic stimulation suppressed OAB contractions in patients.
Neuromodulation has revolutionized the management of OAB and is now well established as a safe and effective treatment for those who don’t respond to conservative medication treatments. Most of this involves uncomfortable and surgically implanted electrical stimulation. PEMFs have been discovered to have similar actions without the discomfort, cost or harm.
NEUROMODULATION
Treatment of OAB should progress from the least to most invasive modality, and neuromodulation is a more attractive option owing to it being a minimally invasive approach, tolerable, having positive outcomes, and being reversible.
Multiple neuroanatomical pathways have been described for sacral neuromodulation including the sacral S3 nerve root, pudendal nerve and tibial nerve. The S3 nerve root is currently the main treatment target and has the most long-term data on safety and efficacy to support its use. However, studies on neuromodulation at the pudendal nerve or posterior tibial nerve have been positive and their role in treatment continues to evolve. Most urologists who are experienced in voiding dysfunction can become proficient in each technique. Patient selection, surgical techniques and postoperative management differ slightly between approaches and urologists should familiarize themselves with these differences.
Neuromodulation has been reported to be effective for the treatment of stress and urgency urinary incontinence. The cure and improvement rates of pelvic floor neuromodulation in urinary incontinence are 30-50% and 60-90%, respectively. In clinical practice, vaginal, anal and surface electrodes are used for external, short-term stimulation, and sacral nerve stimulation for internal, chronic (long-term) stimulation.
The effectiveness of neuromodulation has been verified in a randomized, placebo-controlled study. However, the superiority to other conservative treatments, such as pelvic floor muscle training has not been confirmed. A long-term effect has also been reported. In conclusion, pelvic floor exercise with adjunctive neuromodulation is the mainstay of conservative management for the treatment of stress incontinence. For urgency and mixed stress plus urgency incontinence, neuromodulation may therefore be the treatment of choice as an alternative to drug therapy. (Yamanishi, 2008)
Percutaneous tibial nerve stimulation (PTNS) has been proposed for the treatment of overactive bladder syndrome (OAB), non-obstructive urinary retention (NOUR), neurogenic bladder, paediatric voiding dysfunction and chronic pelvic pain/painful bladder syndrome (CPP/PBS). (Gaziev) Electrical stimulation of the posterior tibial nerve (PTN) has become an established therapy option for the treatment of OAB that failed medical therapy. An implant is surgically placed near the PTN and activated by an external pulse generator. When you have the PTNS treatment a very fine needle (just like an acupuncture needle) is inserted into the lower leg, slightly above the inside of the ankle. This is the area where the tibial nerve runs.
A small pad is stuck to the skin on the bottom of the foot on the same leg. This is a bit like the pads that get stuck on your chest if you have an ECG test. These two electrodes (one needle, one skin-pad) are then connected to the pulse generator which delivers an electrical signal that travels along the tibial nerve up to the sacral nerve plexus in the pelvis. One of the functions of the sacral nerve plexus is to control bladder and pelvic floor function.
When women’s responses to PTNS are compared to standard medication as the only therapy, there are no significant differences in results. Urine leakage associated with a feeling of urgency and loss of stool or gas from the rectum beyond patient’s control became significantly different after treatment in both groups about equally well. (Eftekhar) PTNS was also studied in patients with OAB persisting after 2.5 years of using first-line anticholinergic drugs.
The patients did daily PTNS at home. PTNS was successful following 1 month of treatment in 53% patients. After follow-up at about 10.8 months, 49% continued PTNS. Bladder function scores stayed lower than before treatment. PTNS was considered a second therapeutic option before surgical treatment. (Ammi) Since PTNS is equivalent to medication in its effects, and it is invasive and expensive, it is considered to be 2nd line therapy only, in those who fail medical therapies.
A small number of patients were followed for 9 yrs. Six of the seven patients still had sensory and muscle responses on stimulation at 9-year follow-up. Three of four patients who had a successful treatment response at 1 year, still use the device 9 years later. After 9 years of clinical experience the implant was found to be a safe therapy for OAB.
OAB occurs in patients with other medical conditions. In these situations therapies are much more limited than in the general patient with OAB. When PTNS is compared to pelvic floor muscle training with biofeedback in multiple sclerosis (MS) patients with mild disability, both approaches improve symptoms related to urgency to the same extent. (Gaspard) Pelvic floor muscle training is very time-consuming, expensive and the benefits do not last without continuing some kind of muscle training indefinitely. PTNS was also found to be very helpful in neurogenic OAB after stroke, reducing urinary frequency and urgency.
The long-term efficacy and safety of PTNS for OAB after 3 years from the start of an ongoing course of therapy was established for a particular stimulation system. Patients completed a 36-month program getting 1 treatment per month after an initial 14-week treatment program. 77% maintained moderate or marked improvement in OAB symptoms at 3 years. Voids per day decreased from 12 to 8, nighttime voids decreased from 2.7 to 1.7 and urge incontinence episodes decreased from 3.3 to 0.3 per day. All quality of life parameters remained markedly improved from baseline through 3 years. So, when PTNS is initiated the patient has to commit to long-term therapy with an implanted invasive, electric stimulator.
Another form of stimulation for OAB is another less acceptable invasive approach, vaginal electrical stimulation (ES). ES and PTNS have been compared. ES was applied for 20 min, three times per week for 6-8 weeks with pulses of 10-50 Hz square waves or with 5-10 Hz frequency,. PTNS was applied for 30 min once a week for 12 weeks. Objective tests after both treatments decreased significantly almost to the same extent in each group, but the decrease in the ES group was somewhat greater. The number of patients who describe themselves as cured was higher in the ES group.
The costs and cost-effectiveness of PTNS and sacral nerve stimulation (SNS) have been evaluated. SNS is a more invasive procedure, requiring the insertion of electrodes into the inside of the pelvis. The costs of initial therapy were $1,773 for 12 weekly PTNS treatments. SNS requires an initial evaluation test at $1,857. For ongoing therapy the cost of the SNS surgical implant was $22,970. 2-year maintenance costs were $3,850 for PTNS and $14,160 for SNS, including those who discontinued therapy.
Only 48% and 49%, respectively, remain on therapy at 2 years. PTNS had substantially lower overall cost. Because of the slightly higher rate of success with SNS, an additional 1% of patients would remain on therapy at 2 years if SNS were used rather than PTNS, but the lifetime average cost per patient would be more than $500,000. (Martinson) So, because of concerns about insurance coverage, with a high risk of these costs being mostly borne by the individual patient, there need to be other less expensive alternative therapies available to these very expensive and invasive procedures.
PEMFs may be an ideal neuromodulation alternative to help treat OAB, without the high costs and the need to endure procedures, including tolerating long standing electrical implants in the body.
PEMFS FOR NEUROMODULATION
Neuromodulation also happens with PEMFs, since these magnetic fields reach deep into the body and pelvis non-invasively. Therapeutic electric fields do not go deep into the body. This is why electrical stimulation usually has to be done right on the nerve or muscle being stimulated. That’s also why the stimulators have to be surgically implanted.
PEMFs also have varying abilities to penetrate deep into the body or act on specific nerves or tissues. The deeper in the body the tissue is that needs stimulating the stronger the magnetic field often needs to be. High intensity PEMFs are usually required to do sacral nerve stimulation. High intensity repetitive 15 Hz magnetic stimulation (rMS) was evaluated in women with stress incontinence. rMS of the sacral nerve roots (S2-S4) was applied for 15 mins, 3 days a week for 2 weeks (6 times in all). At 1 week after treatment ended patients in the active stimulation group showed improvement in health perception, social limitation, sleep/energy performance and incontinence severity.
These results were not seen in the sham stimulation group. Also, these results were no longer seen at 1 month after the end of treatment. So, rMS of the sacral roots has a short-term benefit on the quality of life of patients. This is also true as well for electrical stimulation. And, these results are comparable to those seen in short-term treatment programs for pain management using rMS, suggesting that longer-term courses of treatment are necessary. (Manganotti) While this research group did not find significant physical changes with short-term high intensity magnetic stimulation, another group (Fujishiro 2000, Fujishiro 2002) found that with only 30 minutes of treatment with rMS, the number of leaks and amount of urine loss on a pad test significantly decreased with only one treatment session. They also found that there was a 74% improvement in quality of life.
A group of Japanese researchers has worked for years on developing techniques of using magnetic stimulation as part of neuromodulation. They devised a continuous magnetic stimulator allowing longer-term, in office magnetic stimulation, using a magnetic chair type device. They wanted to see if continuous magnetic stimulation would result in strengthening the closing of the urethra when under pressure and inhibition of bladder contractions in dogs. The stimulating coil was placed underneath the pelvis to stimulate the pudendal nerve at 10 Hz. Urethral pressure was increased by more than double and bladder contraction was inhibited. (Yamanishi, 1999) In effect OAB was improved.
HIGH INTENSITY PEMF STIMULATION FOR OAB
In addition to doing neuromodulation, PEMFs may also be able to work on muscle, addressing the myogenic theory and helping with the muscles of the bladder and pelvis itself. In Kegel’s exercises the goal is to stimulate the muscles to contract to reduce incontinence secondary to the lack of muscle strength in the pelvic muscles, affected by the stretching of the tissues during labor, which maintain the position of the bladder in relation to the urethra. When this position is disrupted stress incontinence happens. Kegel exercises frequently fail, for many reasons. As noted above, even stress incontinence can be associated with urge incontinence, partly due to bladder muscle irritability. PEMFs not only strengthen pelvic muscles but also work on the irritable bladder muscles to relax.
An early clinical trial in a small number of women found that magnetic stimulation of the pelvic floor muscles may be effective for urge incontinence, too. (Suzuki) Patients with urge incontinence, who failed pelvic floor muscle training, were given high intensity 10-week PEMF treatments with a continuous 10Hz chair device at about 1100 gauss. They had a number of tests conducted at the end of the 10 week cycle of treatments. This group was compared to another group receiving sham treatments. Magnetic stimulation was found to be effective in reducing urge incontinence in both physical and subjective measures.
In another study by the same group, using 20 Hz 15-minute (with 1-minute on/30-second off cycles) stimulation twice a week for 5 weeks, they studied women with stress incontinence and another group with urge incontinence with magnetic stimulation. In that study, 86% of patients with stress incontinence and 75% with urge incontinence were improved.
The ability of the urethra to control pressure from the bladder to urinate is important in reducing incontinence, to allow some degree of voluntary control, that is, delaying the urge to urinate. In earlier work done by the same Japanese group, they studied the use of a magnetic coil underneath the pelvis in the area from the anus to the pubic bone, called the perineum. They confirmed that urethral pressure increased, suggesting that magnetic stimulation can be effective as a urinary incontinence therapy. (Ishikawa, 1998)
In another study they then looked at the ability of PEMFs to control urethral pressure. An active PEMF treatment group received high intensity functional PEMF stimulation. The stimulating intensity was gradually increased to the tolerable limit. (This is a common approach that we use in the office setting, since individual tolerances tend to vary.) A 15-minute, 20Hz single session was carried out using an on-off cycle of PEMF stimulation. In the active PEMF treatment group, the maximum urethral closure pressure increased significantly after stimulation. In the sham group, no changes were seen. All women tolerated the functional continuous magnetic stimulation well, and none experienced any adverse effect. (Yamanishi, 1999)
In a much larger study to evaluate the efficacy and safety of magnetic stimulation for the treatment of urinary incontinence in women with overactive bladder, a larger group of women with urge incontinence were randomized to active stimulation or sham stimulation. An armchair-type magnetic stimulator was used for 25-minute magnetic stimulation twice a week for 6 weeks, with a magnetic field intensity of 560 mT (5600 gauss) peak at 10 Hz. The sham device only delivered a maximum intensity of 20.4% at 1 Hz.
The number of leaks per week, number of voids/urgency per 24 hours, mean and maximum voided volume, and the quality of life assessment were measured. The active treatment group experienced about half the number of leaks/week and number of urgency sensations/24 hours and a large increase in the amount of urine voided. As for safety, except for rare diarrhea and constipation, no patients experienced any device-related adverse event. (Yamanishi, 2014)
As the above study found, very few adverse events are typically found with PEMF stimulation, even with high intensity PEMFs. To verify this, another group evaluated whether there were any obvious tissue or cycle changes in rats receiving continuous stimulation to their genital organs (uterus and ovaries). The rats underwent 36 sessions of 25-minute PEMF stimulation with 10Hz at a maximum output level of 560 mT (5600 gauss) once per day, 5 days per week. No adverse effects of long-term pulsed magnetic stimulation were noted. Rats are much more sensitive to PEMFs than humans, and because of their high metabolic rate, tend to show adverse effects results sooner than would be seen in humans. So, these results are reassuring to the potential risks to humans of frequent treatment to their pelvic organs with PEMFs to improve OAB and incontinence.
LOW INTENSITY PEMF STIMULATION FOR OAB
While high intensity PEMFs may be very useful to produce short-term benefit for OAB and incontinence, there is always the concern that recurrent courses of treatment may be necessary, potentially for the rest of a woman’s life. As a result, it is useful to know whether lower intensity home-based PEMF systems may be able to produce comparable results.
In one research study, investigators at the University of Maribor in Slovenia, Department of Urogynecology, used a portable magnetic therapy device worn in a garment over the bladder continuously all day. Women with urinary incontinence receiving active device treatment were compared to a group of women who used a non-active sham device. The treatment device had a pulsating magnetic field 10 microTesla and 10Hz frequency, which was worn day and night for 2 months.
Compared with the sham device, the number of pads used was significantly lower, as was the pad weight, and a significant improvement in the power and duration of pelvic floor muscle contractions. Active magnetic stimulation produced a 56% improvement in urinary incontinence symptoms compared with 26% improvement in the sham group. This form of magnetic stimulation is efficient and safe, can be used at home, and because of its small size, wearing the device is not annoying for patients.
In a different study, this group used a similar portable device with 18.5 Hz in women with mixed incontinence and using more objective measures of bladder function. The device was similarly applied: day and night for 2 months. After 2 months of magnetic stimulation there were significant decreases in voiding frequency, nighttime urination and pad use. First sensation of bladder filling and maximum bladder capacity increased significantly before and after stimulation only in the active stimulation group. 78% reported improvement in symptoms after magnetic stimulation with an average success rate 42% versus the sham group at 23%.
The same group looked at the use of this same type of PEMF stimulation in young females with enuresis, or nighttime bedwetting. This relates to women with incontinence, because frequent nighttime urination is a common distress with OAB. Females, mean age 10.8 years, range 6-14 years, were randomly assigned to either active 18.5 Hz magnetic stimulation or sham stimulation.
As above, they wore their stimulators continuously day and night for 2 months. In the active treatment group, the number of weekly enuresis episodes decreased significantly compared to sham, from 3.1 to 1.3 per week. Three girls from the active group were completely dry and four were significantly improved. Also, in the PEMF group there was a significant increase in bladder volume at the time of a strong desire to void as well as an increase in bladder volume at that void.
MAGNETIC VS. ELECTRICAL STIMULATION FOR OAB
As mentioned earlier, much research has been conducted using electrical stimulation as neuromodulation for reducing symptoms of OAB. The challenges with this form stimulation are that it typically is invasive and very uncomfortable and does not allow for home use.
One study was done specifically to compare the two modalities. In that study, an armchair-type device with a local stimulation coil at 10 Hz was applied continuously. Objective measures of improvement were collected. The bladder capacity at the first desire to void and the maximum measured bladder capacity increased significantly during stimulation compared with pre-stimulation levels.
The measured maximum bladder capacity increased significantly more in the magnetic stimulation group by 106% compared with the pretreatment level than that in the electrical stimulation group, which had an increase of only 16%. This is a huge difference. Bladder overactivity was abolished in 3 patients in the magnetic stimulation group but not in any patient in the electrical stimulation group. Although both treatments were effective at some level, the inhibition of bladder overactivity was far greater in the magnetic stimulation group.